Aplastic anemia is a rare and serious blood disorder. It happens when the bone marrow fails to make blood cells. This leads to a lack of red cells, white cells, and platelets. Get 12 key pathophysiology of aplastic anaemia facts. Learn about etiology, blood film, bone marrow, and serious prognosis factors.
It’s very important to act fast when someone has this condition. If not treated, it can be deadly. The disease destroys the cells that make new blood cells. How well someone does depends on how severe it is and how well they respond to treatment.
Knowing how aplastic anemia starts and works is key. It helps doctors diagnose and treat it better.
Aplastic anemia is a condition where the bone marrow doesn’t make enough blood cells. This leads to a lack of red, white blood cells, and platelets. It’s caused by the bone marrow’s failure to produce these cells.
The cause of aplastic anemia is complex. It involves the immune system attacking the bone marrow cells. This shows how important it is to understand the underlying causes.
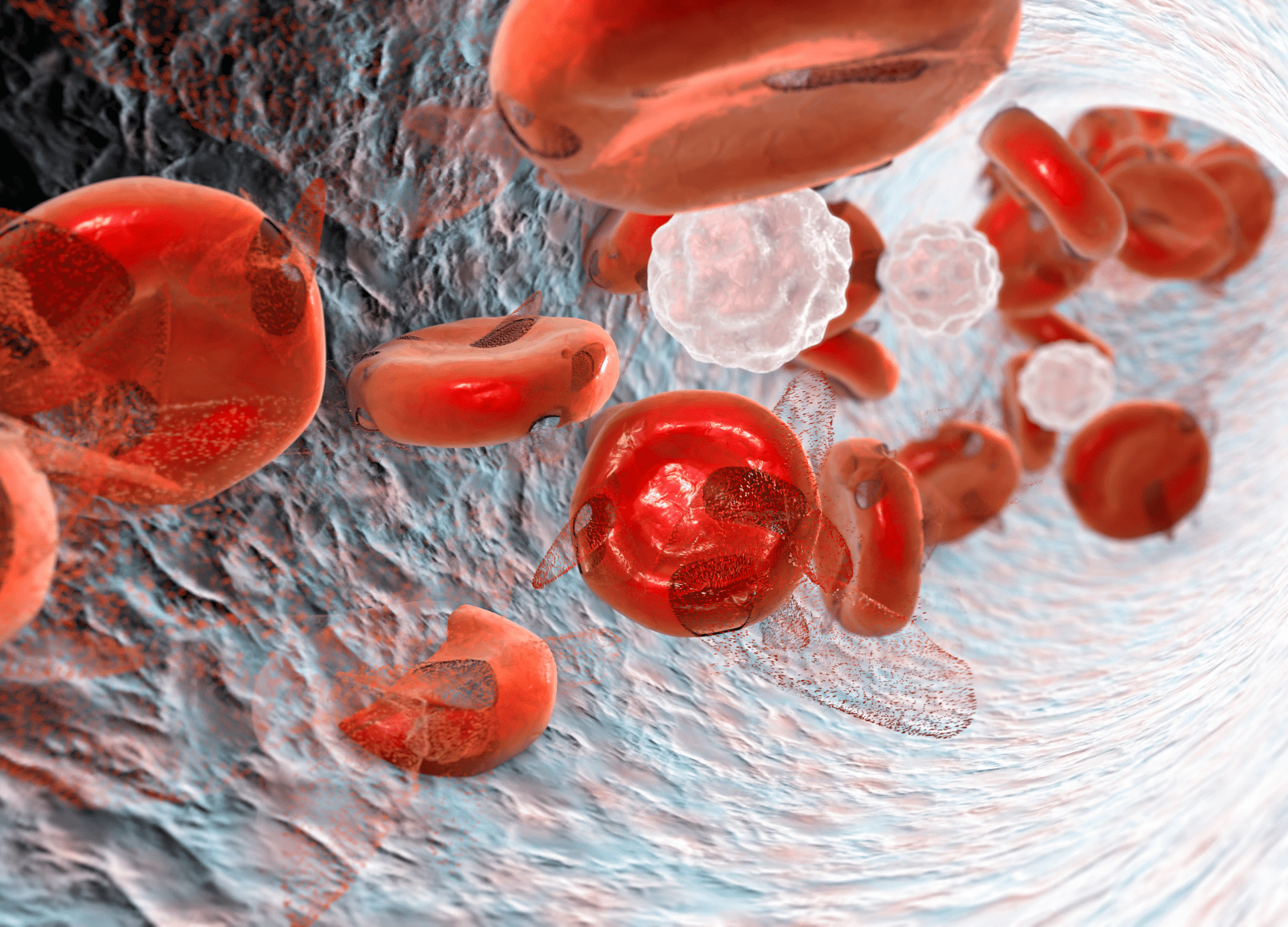
The bone marrow failing to make blood cells is key to aplastic anemia. The bone marrow uses stem cells to create blood cells. But in aplastic anemia, this process is broken, leading to fewer blood cells.
This failure means there are fewer red blood cells, white blood cells, and platelets. This can cause anemia, infections, and bleeding problems.
Pancytopenia is the main sign of aplastic anemia. It means there are fewer red blood cells, white blood cells, and platelets. This can cause tiredness, infections, and bleeding.
Aplastic anemia is rare, and its occurrence varies worldwide. Several factors, like genetics and environment, affect its spread.
Exposure to chemicals, drugs, and radiation can increase the risk. So can viral infections and autoimmune disorders. Knowing these risks helps in early diagnosis and treatment.
“The incidence of aplastic anemia varies geographically, with higher rates observed in Asia compared to Western countries.”
Understanding aplastic anemia’s definition, core concepts, and risks helps in diagnosing and treating it.
Aplastic anemia is caused by a mix of immune attacks and stem cell problems. Knowing how these work is key to finding good treatments.
The immune system is a big part of aplastic anemia. Autoimmune reactions are thought to be the main cause. They make the immune system attack and kill the stem cells in the bone marrow.
Aplastic anemia also has problems with stem cells. These problems are both in how many stem cells there are and how well they work.
These issues mean the body can’t make enough blood cells. This leads to the low blood cell counts seen in aplastic anemia.
The bone marrow’s environment is important for making blood cells. In aplastic anemia, this environment changes in ways that hurt the disease.
These changes make it hard for the bone marrow to help make blood cells. This makes the disease worse.
Understanding how immune attacks, stem cell problems, and changes in the bone marrow work together helps us treat aplastic anemia better.
It’s important to know what causes aplastic anemia to treat it well. This condition happens when the bone marrow can’t make blood cells. This leads to a lack of all blood cell types.
Autoimmune reactions are a big part of aplastic anemia. Here, the immune system attacks the bone marrow’s stem cells. This attack stops the bone marrow from making blood cells, causing a lack of all blood types.
Some viruses can cause aplastic anemia. Viruses like hepatitis, Epstein-Barr, and cytomegalovirus can harm the bone marrow. They do this by directly attacking cells or by triggering an immune response.
Being around certain chemicals or taking some drugs can also cause aplastic anemia. Chemicals like benzene and some pesticides can harm the bone marrow. Drugs like antibiotics and anti-inflammatory medicines can also cause it as a rare side effect. These effects usually happen because the drugs damage the stem cells in the bone marrow.
High doses of radiation can also cause aplastic anemia. Radiation can directly harm the bone marrow, making it less able to make blood cells. The more radiation someone gets, the higher their risk of getting aplastic anemia.
Recent studies have shown that genetics plays a big role in aplastic anemia. This condition is complex, influenced by genes and the environment. Knowing the genetic risks is key to diagnosing and treating it well.
Inherited bone marrow failure syndromes (IBMFS) are rare genetic disorders. They make it hard for the bone marrow to make blood cells. Fanconi anemia is one, linked to aplastic anemia and cancer risk due to DNA repair issues.
“Diagnosing IBMFS needs a detailed genetic check. This includes tests for chromosomal breakage and genetic sequencing to find specific mutations.”
Telomere biology disorders are another genetic factor in aplastic anemia. Telomeres protect chromosome ends, and problems with them can cause bone marrow failure. Dyskeratosis congenita is a disorder linked to aplastic anemia, caused by telomere maintenance gene mutations.
Experts say, “Measuring telomere length is useful in diagnosing aplastic anemia. It’s most helpful in those with a family history of telomere disorders.”
HLA associations are also important in aplastic anemia. Some HLA alleles increase the risk of getting aplastic anemia. This suggests an immune-related part of the disease. Studying HLA can help understand genetic risk and guide treatments.
In conclusion, genetics is key in aplastic anemia. Knowing about inherited syndromes, telomere disorders, and HLA associations is vital. It helps in diagnosing, managing, and possibly preventing aplastic anemia.
The peripheral blood smear is key in diagnosing aplastic anemia. It shows the health of blood cells, helping doctors treat the disease. When looking at a blood film for aplastic anemia, certain features are seen.
Aplastic anemia often shows normocytic or macrocytic anemia. Normocytic anemia means red blood cells are not of normal size. Macrocytic anemia means they are larger than normal. These signs show the bone marrow is not working properly.
Leukopenia, or low white blood cell count, is a key sign of aplastic anemia. This makes it harder for the body to fight off infections. The blood smear shows fewer white blood cells, which is a key finding.
Thrombocytopenia, or low platelet count, is also seen in aplastic anemia. The blood film shows fewer platelets, which can cause bleeding. How low the platelet count is can help doctors understand and treat the condition.
A key feature of aplastic anemia is the absence of abnormal cells. This helps doctors tell it apart from other bone marrow problems. The lack of abnormal cells, along with low counts of all blood cells, confirms aplastic anemia.
In summary, aplastic anemia’s blood smear shows certain signs. These include normocytic or macrocytic anemia, low white and platelet counts, and no abnormal cells. These signs are important for diagnosing and understanding the disease.
Laboratory tests are key to diagnosing aplastic anemia. We use a mix of tests to confirm the diagnosis and understand its severity. These tests check blood and bone marrow.
A complete blood count (CBC) is the first step. It shows blood cell count issues. In aplastic anemia, the CBC often shows pancytopenia, meaning low counts of all blood cells.
The severity of these low counts can differ. But they are often quite low. For example, patients might have severe anemia, neutropenia, and thrombocytopenia. These signs point to bone marrow failure.
Confirming pancytopenia is key to diagnosing aplastic anemia. We do this with CBC results and clinical signs. Pancytopenia is a key sign of aplastic anemia, found through lab tests.
The severity of aplastic anemia is based on pancytopenia levels. We use specific criteria to determine severity. These include the absolute neutrophil count (ANC), platelet count, and reticulocyte count.
| Severity | ANC (cells/μL) | Platelet Count (cells/μL) | Reticulocyte Count (%) |
| Severe | |||
| Very Severe |
To rule out other causes of pancytopenia, we do more tests. These include bone marrow tests, cytogenetic analysis, and tests for infections or autoimmune disorders.
Bone marrow histology gives us key insights into aplastic anemia. It’s vital for diagnosing and understanding how severe the condition is.
In aplastic anemia, the bone marrow shows hypocellular or acellular patterns. This means there’s a big drop in cell numbers. Studies show that how low the cell count is can tell us how severe the anemia is.
One key sign of aplastic anemia is more fat in the bone marrow. As the blood-making cells drop, fat cells take their place. This is seen in biopsies and shows how the marrow is trying to adapt.
Even with low cell counts, some blood-making islands can be found. These islands hint at the marrow’s ability to recover. Knowing about these islands helps doctors predict how well a patient might do.
Bone marrow biopsy is a key test for aplastic anemia. It lets doctors see how many cells there are and what they look like. It’s important to read these results well, as they help confirm the diagnosis and guide treatment.
The outlook for aplastic anemia depends on how bad it is and how well it responds to treatment. Knowing about the bone marrow’s state is key to choosing the right treatment and predicting how well a patient will do.
It’s important to know the signs of aplastic anemia to diagnose and treat it well. This condition happens when the bone marrow fails, affecting blood cells. This failure impacts many types of blood cells.
Anemia is a key sign of aplastic anemia. It causes fatigue, weakness, and shortness of breath. These symptoms make life hard for patients, so they need quick and good care.
At Liv Hospital, we follow strict guidelines to help with these symptoms.
Neutropenia, or low neutrophil count, makes infections more likely in aplastic anemia. We’ll talk about how neutropenia affects patients and how to prevent infections.
| Infection Risk Factors | Prevention Strategies |
| Neutropenia | Prophylactic antibiotics |
| Immunosuppression | Avoidance of live vaccines |
Thrombocytopenia, or low platelet count, can cause bleeding problems. These range from small bruises to serious hemorrhages. It’s key to manage thrombocytopenia well to avoid these issues.
Patients with aplastic anemia face bleeding risks due to thrombocytopenia. This highlights the need for close monitoring and treatment.
Aplastic anemia affects patients’ lives a lot. It impacts their health and mental well-being. We’ll look at how it affects patients overall.
At Liv Hospital, we focus on the whole patient. We aim to improve their quality of life by addressing aplastic anemia’s effects.
Managing aplastic anemia requires a mix of treatments to help the bone marrow work better. Each treatment plan is made just for the patient. It considers how severe the disease is, the patient’s age, and their overall health.
Immunosuppressive therapy is a key treatment for aplastic anemia. It’s used for those who can’t get a bone marrow transplant. This therapy usually includes antithymocyte globulin (ATG) and cyclosporine.
This therapy has helped many patients with aplastic anemia. But not everyone responds the same way. Some might need more treatments.
“Immunosuppressive therapy has revolutionized the treatment of aplastic anemia, giving many patients a better option than bone marrow transplantation.”
Leading Hematologist
Hematopoietic stem cell transplantation (HSCT) is a chance for a cure for aplastic anemia. It’s best for younger patients with a matched sibling donor. The treatment replaces the damaged bone marrow with healthy stem cells from a donor.
| Treatment Modality | Indications | Outcomes |
| HSCT | Younger patients, matched sibling donor | Potential cure, improved survival |
| Immunosuppressive Therapy | Patients not eligible for HSCT | Improved hematologic responses, variable survival |
Supportive care is key in managing aplastic anemia. It aims to ease symptoms, prevent problems, and improve life quality. This includes blood transfusions, preventing infections, and using growth factors.
Supportive care is used alongside treatments like immunosuppressive therapy or HSCT. It’s essential in managing the disease and its side effects.
New treatments for aplastic anemia are being researched. These include new immunosuppressive drugs, gene therapy, and therapies that help the bone marrow work better.
As we learn more about aplastic anemia, new treatments are being developed. These emerging therapies offer hope for better outcomes and more targeted treatments for this complex disease.
The long-term outlook for aplastic anemia depends on how severe the disease is and how well it responds to treatment. Knowing these factors helps doctors manage patients’ hopes and make treatment plans.
Several factors affect aplastic anemia’s prognosis. These include the disease’s severity at diagnosis, how well the patient responds to treatment, and any genetic conditions. Severity at diagnosis is key, with very severe cases having a worse outlook.
The response to treatment is also important. Patients who do well with initial treatments or stem cell transplants tend to do better long-term. Genetic conditions can also influence the prognosis.
Thanks to new treatments, survival rates for aplastic anemia have gone up. Immunosuppressive therapy and hematopoietic stem cell transplantation are the main treatments, each affecting survival differently.
Patients getting stem cells from a matched sibling often have high survival rates, sometimes over 80-90%. Immunosuppressive therapy is also effective, mainly for those without a donor, with survival rates depending on the treatment and patient response.
Even with better survival rates, aplastic anemia patients face long-term risks. These include relapse of the disease, secondary malignancies, and late effects of treatment like organ damage.
It’s vital to keep an eye on these complications over time. Regular check-ups with a hematologist/oncologist are key. All we watch for are secondary cancers and organ function, mainly for those who had stem cell transplants.
Our knowledge about aplastic anemia has grown, leading to better care for patients. Doctors now understand the disease’s causes and symptoms better. This helps them diagnose and treat it more effectively.
Studies have shown how aplastic anemia affects the bone marrow. This knowledge has helped create new treatments. These include medicines that reduce the immune system’s attack and stem cell transplants.
Dealing with aplastic anemia needs a team effort. This includes supportive care and new treatments. As we learn more, we’ll find even better ways to help patients.
By improving how we understand and treat aplastic anemia, we can make patients’ lives better. This means they can live longer and have a better quality of life.
Aplastic anemia is a serious blood disorder. It happens when the bone marrow fails to make blood cells. This leads to a lack of red, white blood cells, and platelets.
Many things can cause aplastic anemia. This includes autoimmune attacks, viral infections, and drug side effects. Also, radiation and genetic issues like inherited bone marrow failure can play a role.
Symptoms include feeling tired, weak, and short of breath. You might also get sick more easily and bleed a lot. These problems can really affect your life.
Doctors use several tests to diagnose aplastic anemia. They look at your blood, do a bone marrow biopsy, and run other tests. This helps figure out if you have it.
A bone marrow biopsy is key in diagnosing aplastic anemia. It shows if the marrow is empty or full. It also helps rule out other diseases.
Treatment for aplastic anemia includes medicines to boost the bone marrow. Sometimes, a stem cell transplant is needed. Supportive care, like blood transfusions, is also used.
The outlook for aplastic anemia patients varies. It depends on how severe the disease is and how well you respond to treatment. Survival rates differ based on the treatment.
Some patients can be cured with the right treatment, like a stem cell transplant. But others need ongoing care to manage their condition.
Long-term issues include the chance of the disease coming back. There’s also a risk of getting other cancers and organ damage. Long-term monitoring is needed.
Aplastic anemia can greatly lower your quality of life. Symptoms like anemia, infections, and bleeding make it hard to live normally. The emotional toll of dealing with a chronic illness is also significant.
References:
Have questions or need assistance? Our team is here to help you with appointments, services, or general inquiries.